Centre for Environmental Health and Sustainability
Knowledge Mobilisation
Knowledge Mobilisation Lead: Dr Joshua Vande Hey
Introduction to knowledge mobilisation

Knowledge mobilisation is about bringing together different communities to share knowledge and promote change.
Knowledge mobilisation is a two-way process that enables advances in health protection research to create benefits for patients and the public. It promotes research that is informed by policy makers, public health practitioners, the public, and other stakeholders to produce outputs which consider many different points of view.
Effective knowledge mobilisation involves:
- Researchers who engage with the policy, practice, research and public communities where their research can make a difference, as part of devising their research questions, to ensure that they address important questions in a useful way
- Researchers influencing decision-making processes in policy, practice and elsewhere through having a 'seat at the table' alongside other approaches to dissemination
- Increasing understanding of the value of research, including limitations, among those who can use research findings.
Knowledge mobilization is an iterative process, using continual stakeholder feedback to guide research goals.
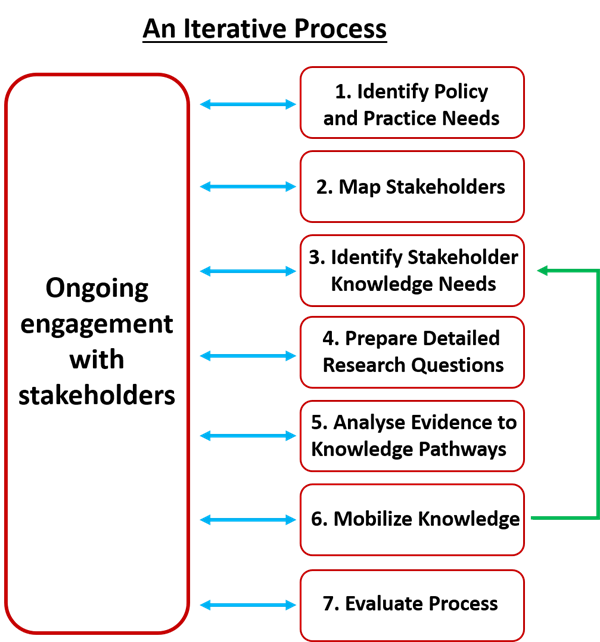
The steps involved in knowledge mobilisation are:
- Identify overarching policy/practice needs
- Map key stakeholders
- Meet with key stakeholders to understand their evidence and knowledge gaps and the nature and format of evidence needed
- Work with science teams to formulate research questions and study designs to address evidence gaps
- As preliminary results emerge, consider process for moving from generating evidence to embedding knowledge
- Mobilise knowledge: Generate policy briefs, SOPs & good practice guides, public facing press releases, practitioner training
- Evaluate impact and effectiveness of KM including through stakeholder feedback
Engagement with wider policy-makers, professionals, industry and the public
We aim to produce KM outputs that are in the most relevant format for the target audience(s) and taking into considering their needs and the range of actions options for change available to them. The knowledge mobilisation undertaken considers impacts and concerns around health inequalities across the work of the HPRU.
Identification of stakeholders
Stakeholder mapping analysis is maintained and updated to identify specific, relevant and impactful target groups for the HPRU as well as for each project throughout the 5 years of the programme. This considers the influence of stakeholders and stakeholder interest, which helps us determine the level of engagement necessary.
We are adapting the level of engagement appropriately to the stakeholder and the topic, as some stakeholders require only occasional dissemination-type engagement and others require specific dialogue and collaboration. We identify and engage stakeholder groups beyond those who typically have a seat at the table.
Example stakeholders include but are not limited to those listed below.
- Learned societies and professional organisations
- Other researchers
- National and local government
- Clinicians and health care professionals
- Public communities
- Industry
KM in action: Discussing and demonstrating 3D printers as part of the Indoor Air and Health HPRU project.