Targeting toxins
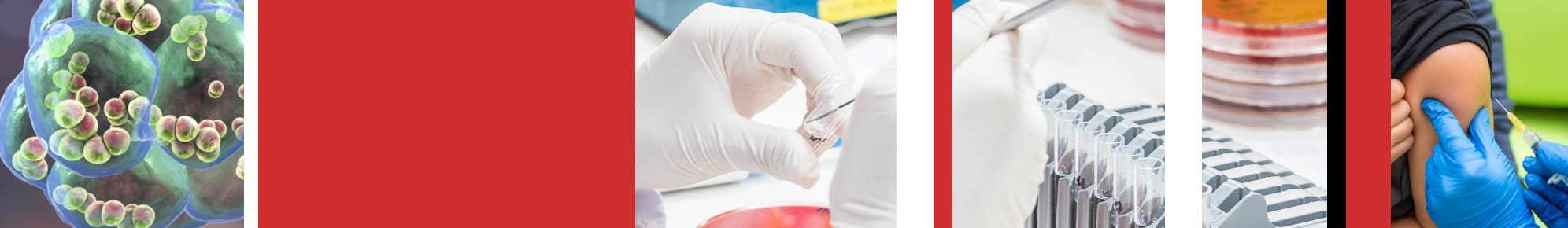
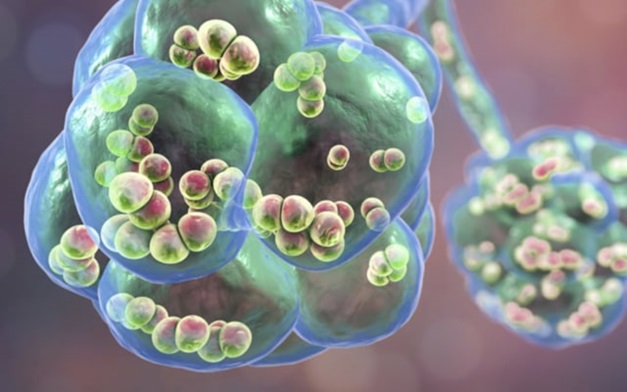
If you are unlucky enough to develop bacterial pneumonia, the bacterium in question will probably be Streptococcus pneumoniae (aka the ‘pneumococcus’), a nasty microbe that can also cause meningitis, septicaemia, otitis media and other serious conditions. The particular factor which enables pneumococcus to attack mammalian cells is a toxin called pneumolysin which is capable of disrupting cell mechanisms by creating pores in membranes. The World Health Organisation estimates that 1.6 million people die each year from pneumococcal infections. Cryo-EM, a rapidly advancing form of electron microscopy conducted at very low temperatures, had already revealed the circular structure, 30-50 molecules in size, which builds up on the membrane and creates the pore. This structure has been visualised at a resolution of about 28 angstroms (one angstrom is a ten-billionth of a metre or 10-10m) but that’s not sufficient to view a single molecule of pneumolysin and ascertain the mechanism by which it binds to the membrane in the first place. It is the possibility of disrupting or preventing that initial binding which holds a key to targeting pneumolysin and hence the pneumococcus.
In 2015 a team led by Professor Peter Andrew and Professor Russell Wallis from our Department of Respiratory Sciences used X-ray crystallography to study pneumolysin at an eye-watering resolution of just 1.98 angstroms and from this they were able to achieve the long-sought goal of determining its molecular structure.
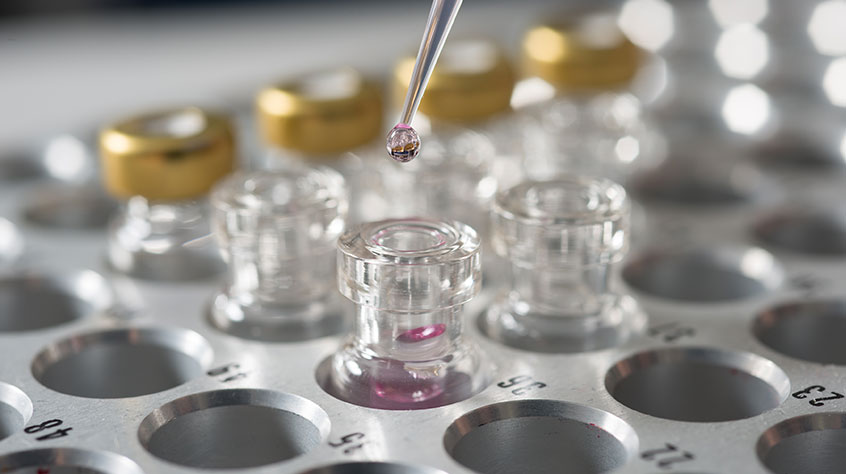
The first stage of the process was to grow a crystal of pneumolysin. The toxin was extracted, purified and filtered then grown in a protein substrate. A second crystal was grown of just one of the molecule’s four parts or ‘domains’; Domain 4 was already known to have the membrane-binding mechanism.
Determining the molecular structure required a trip to Diamond Light Source, the UK's national synchrotron science facility. In this Oxfordshire particle accelerator the crystals were blasted with X-rays, producing distinctive diffraction patterns. Analysing those patterns is what led the Leicester team to their great breakthrough.
The implications of this research are potentially enormous. As the world approaches a post-antibiotic era, medicine will increasingly rely on being able to target the precise interactions of molecules: fighting disease with a sabre rather than a cudgel. There is still a great deal of work to do in finding a way to prevent pneumolysin from binding to membranes, but the first step – finding out how that binding occurs at the level of molecular structures, has been taken.
The implications of this research are potentially enormous. As the world approaches a post-antibiotic era, medicine will increasingly rely on being able to target the precise interactions of molecules: fighting disease with a sabre rather than a cudgel. There is still a great deal of work to do in finding a way to prevent pneumolysin from binding to membranes, but the first step – finding out how that binding occurs at the level of molecular structures, has been taken.
Much of the experimental work involved in this breakthrough was carried out by PhD students Jamie Marshall and Bayan Faraj from our Department of Infection, Immunity and Inflammation. Also contributing to the work were Rana Lonnen and Md Arif Sheikh from the same department, and Alexandre Gingras, Mohammed El-Mezgueldi and Peter Moody from our Department of Molecular and Cell Biology. The work was funded by the Wellcome Trust and the Medical Research Council and was published in the journal Scientific Reports.